TL;DR: After stopping antidepressants, the brain can gradually adjust back to its pre-medication state, but this process and its outcomes can vary significantly between individuals. Some people may return to their previous mental state, while others may experience lasting changes or improvements.
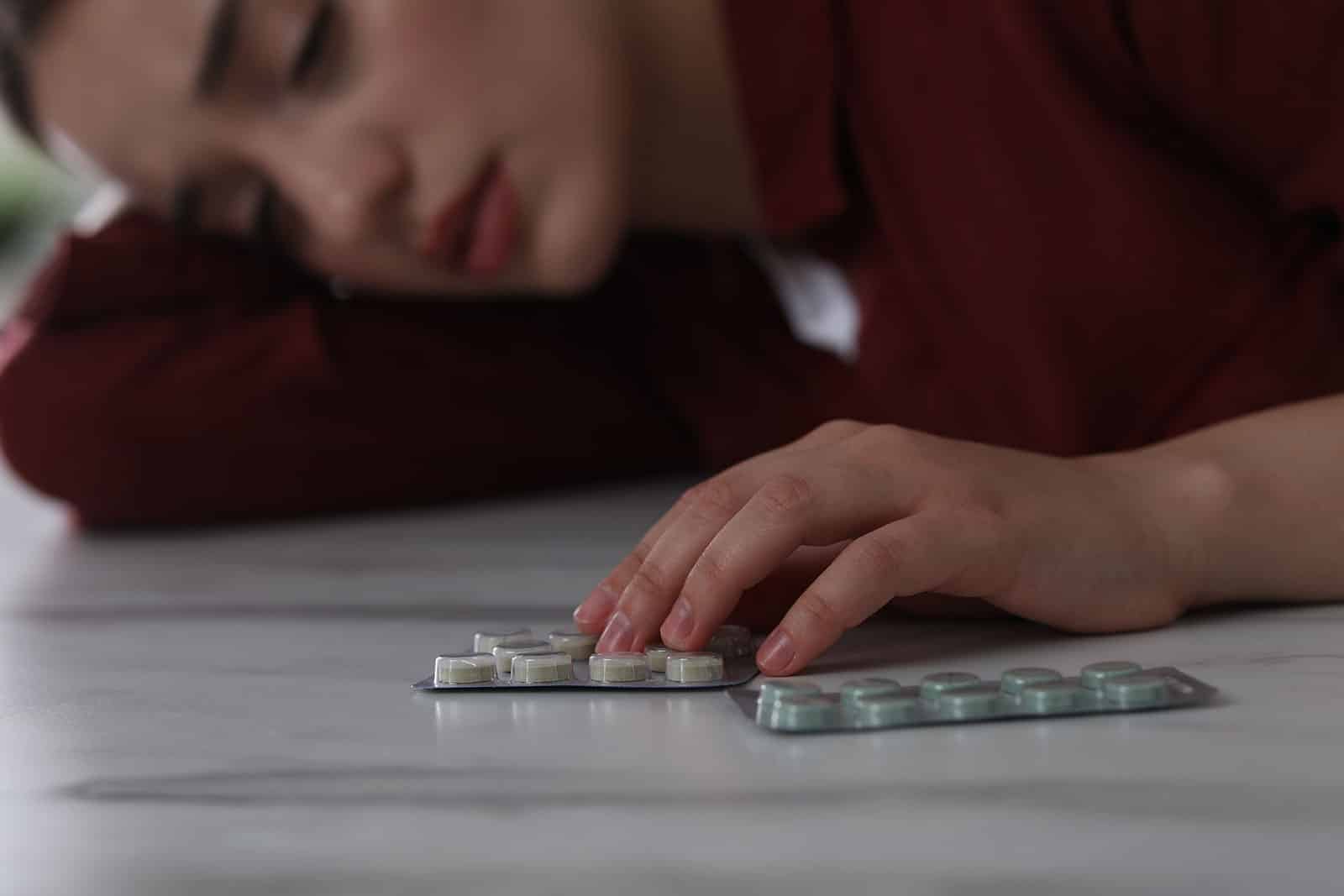
Severe depression, or other depressive disorders in general, is a prevalent mental illness disorder affecting millions worldwide, significantly impacting their emotional well-being, daily functioning, and overall quality of life. Characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities, the debilitating condition often requires a comprehensive approach to treatment.
The treatment involves the use of antidepressant medication, which plays a crucial role in alleviating symptoms of depression by restoring the balance of neurotransmitters in the brain, thus helping individuals regain control over their lives. These medications, however, are not without controversy. The long-term use effects and the process of discontinuing them raise concerns about whether the brain can return to its normal state afterward.

On the same note, research also suggests that the human body possesses a remarkable ability to adapt and recover from these alterations. When a person decides to stopping antidepressant usage, they may experience antidepressant withdrawal symptoms as their body attempts to recalibrate. With perseverance, support, and the natural resilience of the body, it’s possible for an individual to regain their equilibrium and, for the most part, return to their normal state of functioning.
To answer if our brain goes back to normal after taking antidepressants, let’s take a closer look at the role of antidepressants, their influence on the brain, and the impact of the treatment methods on our physical as well as mental well-being.
Table of Contents
Understanding Antidepressants
Antidepressant drugs work by altering the levels of certain neurotransmitters in the brain, helping to restore balance and improve mood. Following are some common types of antidepressants:
Different types of antidepressants and their mechanisms of action
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are the most commonly prescribed class of antidepressants. They work by increasing levels of serotonin, a neurotransmitter that contributes to feelings of well-being and happiness in the brain. SSRIs accomplish this by blocking the reabsorption of serotonin by neurons, thereby making more of it available in the synaptic cleft. Some common SSRIs include fluoxetine (Prozac), sertraline (Zoloft), and escitalopram (Lexapro).
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
SNRIs are somewhat similar to SSRIs but also target norepinephrine – another neurotransmitter involved in mood regulation. These inhibitors alleviate depressive symptoms by increasing the levels of both serotonin and norepinephrine. Examples of SNRIs are venlafaxine (Effexor), duloxetine (Cymbalta), and desvenlafaxine (Pristiq).
Tricyclic antidepressants (TCAs)
TCAs are an older class of antidepressants that, like SNRIs, target both serotonin and norepinephrine. However, they also affect other neurotransmitters and receptors, leading to a broader range of side effects. Due to their side effect profile, TCAs are generally prescribed only when other options have proven ineffective. Types of TCAs include amitriptyline (Elavil), nortriptyline (Pamelor), and imipramine (Tofranil).
Monoamine oxidase inhibitors (MAOIs)
MAOIs are yet another older class of antidepressants work by inhibiting the activity of monoamine oxidase, an enzyme responsible for breaking down neurotransmitters like serotonin, norepinephrine, and dopamine. This leads to increased levels of these neurotransmitters in the brain. MAOIs are typically reserved for treatment-resistant cases due to their potential for serious drug and food interactions. Common MAOIs include phenelzine (Nardil) and tranylcypromine (Parnate).

Factors that influence the effectiveness of antidepressants
Not all antidepressant treatments yield the same results because factors like treatment duration, dosage, and individual responses play a significant role in responding to the treatment. Understanding these factors is crucial to optimizing one’s mental health journey.
Duration of treatment
Antidepressants often require several weeks to reach their full therapeutic effect. Therefore, patients need to continue taking their medication as prescribed, even if they do not notice immediate improvements in their symptoms.
Dosage
The optimal dosage of an antidepressant varies from person to person. Physicians typically start patients on a lower dose and gradually increase it as needed to minimize side effects and determine the most effective dosage.
Individual response and side effects
Each person’s response to an antidepressant is unique, and it may take some trial and error to find the most suitable medication for an individual. Side effects can also vary and may include dizziness, nausea, weight gain, flu-like symptoms, or sexual dysfunction. Accordingly, patients must communicate any side effects or concerns to their healthcare provider, who can help adjust the treatment plan as needed.
The Brain’s Adaptation to Antidepressants
As already mentioned, the human brain has a remarkable capacity to adjust and adapt to the effects of medications. Key aspects of this adaptation process include neuroplasticity, alterations in neurotransmitter levels, and the influence of genetic factors on antidepressant response. Here’s a brief look at how the brain adapts to antidepressants:
- Neuroplasticity is the brain’s inherent ability to change its structure and function in adapting to antidepressant treatment. This dynamic process allows the brain to form new neural connections, modify existing ones, and even create new neurons, which can help alleviate depressive symptoms and improve overall mental health.
- When a person takes antidepressants, the medication affects the brain’s neurotransmitter levels, specifically serotonin and norepinephrine. As the brain adapts to these changes, it adjusts the sensitivity of the receptors and the production of neurotransmitters to maintain balance. This demonstrates the brain’s amazing ability to adapt and respond to the presence of antidepressants, ensuring their effectiveness in regulating mood and improving mental health.
- The brain’s adaptation to the influence of antidepressants is not only a matter of neurotransmitter levels and receptor sensitivity but also involves genetic factors. Each individual possesses unique genetic variations that can impact how they respond to antidepressant treatment. These genetic differences may affect neurotransmitter synthesis, metabolism, and receptor function, ultimately shaping how the brain adapts to the medication.
The Process of Discontinuing Antidepressants
Antidepressant discontinuation syndrome (ADS) is a process that requires careful planning and support to ensure a smooth transition and minimize withdrawal effects. Since the transition is a gradual process, medical therapy centers use tapering and various support strategies to help their patients get back to normal life.

A. Tapering off antidepressants is crucial to minimize withdrawal symptoms that may arise when stopping the medication abruptly. This process typically involves gradually reducing the dose under a healthcare provider’s guidance, allowing the brain to adjust to the changing levels of neurotransmitters. The tapering schedule may vary depending on the specific antidepressant, the dosage, and the individual’s response to the medication.
B. Alongside the tapering process, several strategies can be employed to support brain health and overall well-being during and after discontinuation. These include:
- Psychological support and therapy: Engaging in treatment, such as cognitive-behavioral therapy (CBT) psychotherapy or other forms of counseling, can provide valuable emotional support and equip individuals with coping mechanisms to manage potential mood fluctuations during the discontinuation process.
- Healthy lifestyle habits: Maintaining a healthy lifestyle is essential for overall brain health. Regular exercise, a balanced diet, and adequate sleep can all contribute to improved mental well-being and help mitigate potential withdrawal symptoms.
- Alternative and complementary treatments: Exploring alternative and complementary treatments, such as meditation, acupuncture, or yoga, can offer additional support during the discontinuation process.
What Happens to the Brain After Discontinuing Antidepressants?
Research on brain function and structure after discontinuing antidepressants is an ongoing area of study. Some studies suggest that the brain may undergo a period of readjustment, during which neurotransmitter levels and receptor sensitivity gradually return to their pre-treatment state. However, more research is needed to fully understand the long-term implications of antidepressant discontinuation on brain function and structure.
Factors that influence the brain’s return to normal functioning
Despite the endless research to find answers, we know for sure that certain will play a critical role in controlling the brain after antidepressants are discontinued. These factors are:
- Duration of antidepressant use: The length of time a person has been taking antidepressants can impact the brain’s ability to readjust. Longer durations of use may require more time for the brain to regain its equilibrium.
- Individual biology and genetics: Each person’s unique biology and genetic makeup can influence how their brain responds to discontinuing antidepressants. Variations in genes related to neurotransmitter synthesis, metabolism, and receptor function can impact the brain’s adaptability and the overall recovery process.
- Environmental factors and stressors: External factors, such as stress, social support, and lifestyle choices, can also affect the brain’s ability to return to normal functioning. A supportive environment and healthy lifestyle habits can help promote a smoother transition and facilitate recovery.
It’s important to understand that the brain’s journey to normalization is a complex and multifaceted process. After discontinuing antidepressants, the brain undergoes a readjustment period as neurotransmitter levels and receptor sensitivity gradually return to their pre-treatment state.
What’s Next!
Given the complexity of this transition, it’s essential to prioritize personalized treatment plans and continuous monitoring to support optimal mental health outcomes and ease the pathway for individuals discontinuing their medication.
Don’t settle for a one-size-fits-all approach to drug rehab. At Live Free Recovery Services in New Hampshire, we prioritize addressing all your needs for a safe, long-term recovery from drug and alcohol addiction, not just a cold turkey but proper healthcare. Experience our client-focused care firsthand – contact us now!
FAQ
What is the length of time in which side effects have been seen after stopping the Antidepressants?
What happens to the brain when taking antidepressants?
Does the brain return to its normal state after stopping antidepressants?
Can there be withdrawal symptoms after stopping antidepressants?
How long does it take for the brain to return to normal after stopping antidepressants?
Will my depression or anxiety return after stopping antidepressants?
Can I stop taking antidepressants abruptly?
How can I maintain my mental health after stopping antidepressants?
What are the long-term effects of using antidepressants?
Can antidepressants cause permanent changes to the brain?
How do I know if it’s the right time to stop taking antidepressants?
Published on: 2023-04-19
Updated on: 2024-04-11
